Genetic sequence data for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes Coronavirus Disease 2019 (COVID-19), has played a critical role in the public health response, including in the design of diagnostics and vaccines. Within the Department of Defense, SARS-CoV-2 genetic sequence data plays a vital role in force health protection efforts.
The Armed Forces Health Surveillance Branch’s Global Emerging Infections Surveillance (GEIS) section fostered collaboration with its existing partnerships with Army, Navy, and Air Force public health and medical research laboratories to leverage DoD’s SARS-CoV-2 sequencing efforts. Sequence data from this collaboration will provide critical information about transmission patterns, track diagnostic effectiveness, and guide the development and evaluation of medical countermeasures for the 1.4 million active duty and 331,000 reserve personnel.
“GEIS-funded surveillance provides near-real time understanding of how the SARS-CoV-2 virus is evolving. This information is critical for the development of a vaccine and treatment,” stated Navy Capt. Guillermo Pimentel, GEIS chief. “Previous investments by GEIS in this technology have given our partners the capability to respond and sequence SARS-CoV-2 genomes isolated from DoD Service members around the world.”
In 2017, GEIS established a Next Generation Sequencing and Bioinformatics Consortium to work with GEIS partner DoD laboratories to coordinate and improve pathogen sequencing and analysis efforts around the world. Consortium partners can rapidly detect and characterize known, emerging, and novel infectious disease agents using data from pathogen sequencing. This helps to inform force health protection decision making. The core Consortium partners include: the Naval Medical Research Center (NMRC), U.S. Army Medical Research Institute of Infectious Diseases, Walter Reed Army Institute of Research, U.S. Air Force School of Aerospace Medicine, and the Naval Health Research Center.
“We have used virus sequence data in numerous studies to track virus transmission [such as dengue and influenza],” said Irina Maljkovic Berry, chief of Viral Genetics and Emerging Diseases for the WRAIR Viral Diseases Branch in Silver Spring, Maryland. “We estimate outbreak origins to detect and track vaccine escape and other important mutations throughout the world to aid in vaccine design.”
Consortium partners played a key role in analyzing previous viral outbreaks, such as Ebola in West Africa and Zika in South America, and in seasonal influenza vaccine selection. “Each year we generate thousands of influenza genomes that we use to determine how influenza is evolving or evading our vaccines which directly impact our forces,” said Clarise Starr, deputy chief of Pathogen Detection and Therapeutics Portfolio Applied Technology and Genomics Division, U.S. Air Force School of Aerospace Medicine. “These efforts will be the same essential practices that we’ll need to deploy in response to SARS-CoV-2.”
This open partnership and investment proved extremely helpful in response to the COVID-19 pandemic. DoD laboratories quickly established the ability to isolate the virus, share samples, and compare laboratory methods to improve their sequencing capabilities. “We have been evaluating a few different laboratory sequencing protocols to determine which one works best for samples with certain attributes, in order help increase the efficiency of SARS-CoV-2 sequencing from swabs,” according to Kimberly Bishop-Lilly, head of Genomics & Bioinformatics Department at NMRC in Fort Detrick, Maryland.
The sequence data that’s being collected is a valuable source of information to better understand virus transmission patterns among DoD personnel, particularly when combined with other clinical and epidemiological data. These data are also compared to global virus sequence data.
“The goal is to have data and information that could help answer how local outbreaks may have started, how SARS-CoV-2 may have spread in a community or geographic area, and how we can better contain spread or improve interventions,” said Lindsay Morton, GEIS’s senior molecular epidemiologist. Thus far, SARS-CoV-2 sequence data has been gathered from infected personnel at more than 25 locations across the globe.
Additionally, GEIS partners are leveraging this technology to improve understanding of global circulation of SARS-CoV-2 through surveillance programs at DoD overseas labs, such as in Thailand, Peru, Kenya, and Cambodia.
“The OCONUS (Outside Continental United States) labs are starting to stand up SARS-CoV-2 sequencing capabilities and the core labs of the Consortium are providing them reach-back support for sequencing protocols and for bioinformatics analyses,” said Bishop-Lilly. “Consensus viral genomes are being produced at some of the OCONUS labs and we are comparing to viral genomes obtained from samples in other regions such as the U.S., to identify what lineage is predominant in a given geographic region and what key genetic variations may be predominant in a certain area.”
These data will provide a better understanding of transmission in these locations and result in a better understanding of risk to U.S. forces deployed around the world as the COVID-19 pandemic continues. GEIS leaders hope that increased collaboration across the agencies will propel the research and production of an effective vaccine.
“The key to fully utilizing SARS-CoV-2 sequence data is collaboration,” said Morton, “Consortium partners are ready and willing to engage with organizations involved with clinical studies and outbreak investigations across the DoD to better guide the Department’s response to COVID-19 and reduce the impact to readiness and operations around the world.”
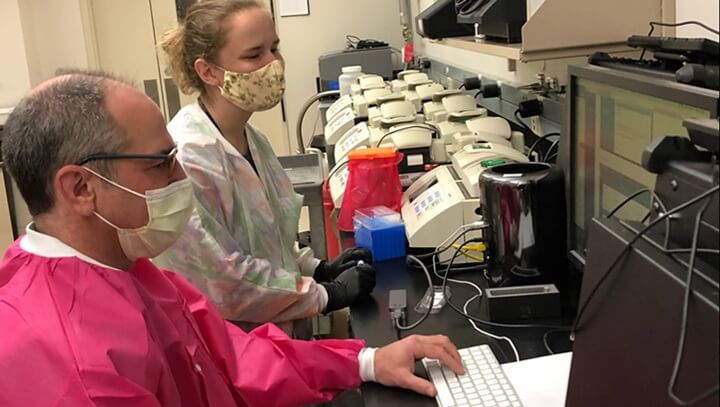
Photo: Research associate Lindsay Glang and senior bioinformatics analyst Gregory Rice sequencing SARS-CoV-2 genomes on Oxford Nanopore MinION platform at NMRC BDRD. Photo Courtesy of Naval Medical Research Center, Genomics & Bioinformatics Department.