The approval in 2018 of a new drug to treat polyneuropathy caused by a rare and frequently fatal disease called hereditary transthyretin-mediated amyloidosis (hATTR) marks the arrival of a new class of therapeutics.
The new drug, called patisiran (Onpattro), is a small interfering RNA (siRNA) that is part of a class of therapeutics that can target hereditary diseases by affecting gene function. With this ability to target specific RNA “messages,” we now have the potential to design therapeutics for a wide range of diseases. Patisiran is the first drug approved to treat hATTR.
According to Data Bridge Market Research, RNA therapeutic drugs exert their effect by silencing a portion of RNA through the use of short interfering RNAs (siRNAs) or microRNAs (miRNAs) involved in causing the disease. RNA-based therapies such as antisense, siRNAs, aptamers, microRNA mimics/anti-miRs and synthetic mRNA have potential to treat a variety of chronic and rare diseases.
What Causes hATTR?
Under normal circumstances, the liver produces a protein called transthyretin (TTR), which is used to transport vitamin A and a thyroid-binding protein in the body. People with hATTR have a mutation in the gene for TTR, which means that the TTR protein manufactured by the liver is defective and unstable. The unstable protein can degrade to form smaller “misfolded” proteins, which can form deposits, or plaques, in the body’s tissues over time. These deposits are called amyloid and tend to build up, mainly in the nerves and heart, but in other tissues as well. They can lead to muscle atrophy, neuropathy, and other devastating symptoms.
How does this class of drugs work?
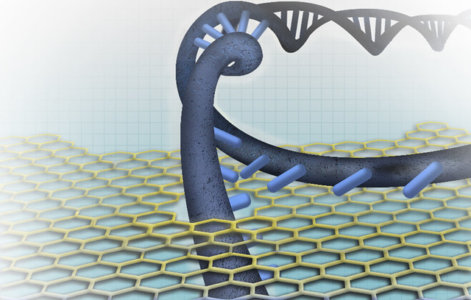
siRNAs belong to a class of drugs known as oligonucleotides that work inside the cell at the RNA level. siRNAs are composed of two complimentary RNA strands (sense and antisense). The antisense strand is designed to target a complimentary strand of mRNA inside the cell and degrade, or “silence” it. siRNAs can alter or stop the production of disease-causing proteins by harnessing RNA interference (RNAi), a process that occurs naturally within our cells. RNAi was first discovered by Craig Cameron Mello and Andrew Fire, who won the 2006 Nobel prize for Physiology and Medicine for their groundbreaking work.
This ability to degrade or “silence” mRNA is especially important for certain rare genetic diseases, including hATTR. Patisiran binds to the TTR mRNA sequence and uses a naturally occurring process to cut it, halting the production of the misfolded proteins. Clinical studies have found that patisiran can reduce the amount of misfolded protein production by 80-85 percent.
Why are these drugs unique?
This class of drugs is unique because the drugs work at the RNA level to specifically silence the production of a disease-causing protein. siRNAs can be designed to interfere with the production of abnormal proteins throughout the body, and are often chemically modified to ensure they are not destroyed by enzymes in the body.
These drugs also require a delivery system such as a lipid nanoparticle to get the drug to specific target tissues. Patisiran is encased in a lipid nanoparticle, which carries and delivers the drug to the liver, but this carrier molecule can trigger its own immune response. Therefore, before taking patisiran, which is administered through an intravenous infusion, patients must take a steroid, acetaminophen, and antihistamines to decrease the chance of having immune reactions. Additional research is underway to design a drug delivery system that can reach target tissue without causing an immune response.
What’s Next?
Initially focused on infectious diseases and oncology, this technology is now being applied across many therapeutic areas, including dermatology, neurology, cardiology, nephrology, and pulmonology. Additional RNAi drugs that focus on rare diseases of unmet medical need are also in the pipeline, especially those for which we understand the underlying genetic cause. FDA anticipates that this is the beginning of a new and exciting generation of therapeutics.